Treatment of Periodontitis

Treatment of Periodontitis
Periodontitis is an advanced stage of gingivitis characterized by inflammation of the gums and damage to the structures that support the teeth, including bone. If left untreated, it can lead to tooth loss and other oral health complications.
Periodontitis is primarily caused by the buildup of plaque, a sticky film of bacteria, on the teeth and gums. The bacteria in the plaque release toxins that irritate and inflame the gum tissues, causing them to pull away from the teeth. Over time, plaque hardens into tartar, which further contributes to the progression of periodontitis.
Causes and risk factors of periodontitis
Periodontitis can be caused by a number of factors, including poor oral hygiene, smoking, genetic predisposition, certain medical conditions such as diabetes, hormonal changes, and certain medications. Poor oral hygiene is one of the main culprits, as insufficient brushing and flossing allow plaque to build up and harden into tartar. Smoking also increases the risk of periodontitis, as it affects the body's immune response and reduces blood flow to the gums.
Forms of periodontitis
Chronic periodontitis: Chronic periodontitis is the most common form of periodontitis. It develops slowly over time and is usually seen in adults. Symptoms of chronic periodontitis can include swollen and red gums, receding gums, bad breath, and the formation of deep pockets between the teeth and gums. These pockets allow bacteria to accumulate and further damage the tissues and bones that support the teeth. Left untreated, chronic periodontitis can lead to tooth loss.
Aggressive periodontitis: Aggressive periodontitis is a more severe form of periodontitis that affects people at a young age. It develops quickly and can be a challenge to treat. Aggressive periodontitis is characterized by the destruction of gum tissue and bone, leading to tooth loss. Symptoms can include inflamed gums, loose teeth, and plaque and tartar buildup.
Necrotic diseases of the periodontium: Necrotizing periodontal diseases are characterized by tissue death in the gums, periodontal ligament and alveolar bone. This form of periodontitis can be extremely painful and is often associated with other factors such as stress, smoking, malnutrition and underlying conditions such as HIV/AIDS. Symptoms can include severe gum pain, bleeding, sore gums and bad breath. Immediate treatment is essential to prevent further tissue damage and tooth loss.


Periodontitis as a manifestation of systemic diseases: Periodontitis can also appear as event systemic diseases such as diabetes, heart disease and respiratory disease. The bacteria and inflammation associated with periodontitis can worsen these underlying health problems and vice versa. It is important for people with systemic diseases to maintain good oral hygiene and seek regular dental care to prevent the progression of periodontitis and its effects on overall health.
Periodontitis associated with endodontic lesions: Endodontic lesions refer to infections or inflammations within the tooth pulp and root canal system. In some cases, these endodontic lesions may contribute to the development of periodontitis. Bacteria from the infected tooth can spread to the surrounding gum tissues, leading to inflammation and damage. Correct diagnosis and treatment of both endodontic damage and periodontitis are essential to achieve successful results.
Symptoms and signs of periodontitis
Recognizing the symptoms and signs of periodontitis is crucial for early detection and treatment. Common signs include swollen, red and tender gums, bleeding gums, persistent bad breath, receding gums, loose teeth and changes in the way your teeth fit together when you bite. It is important to note that periodontitis can be painless in its early stages, which is why regular dental check-ups are essential for early diagnosis.
Stages of periodontitis
Periodontitis develops in several stages, each with its own characteristics and severity. The initial stage is gingivitis, which is characterized by inflamed gums that bleed easily. If left untreated, gingivitis can progress to periodontitis, where the gums pull away from the teeth, forming pockets that become infected. As the infection spreads, the supporting bones and connective tissues are destroyed, leading to tooth loss.
Diagnosis of periodontitis
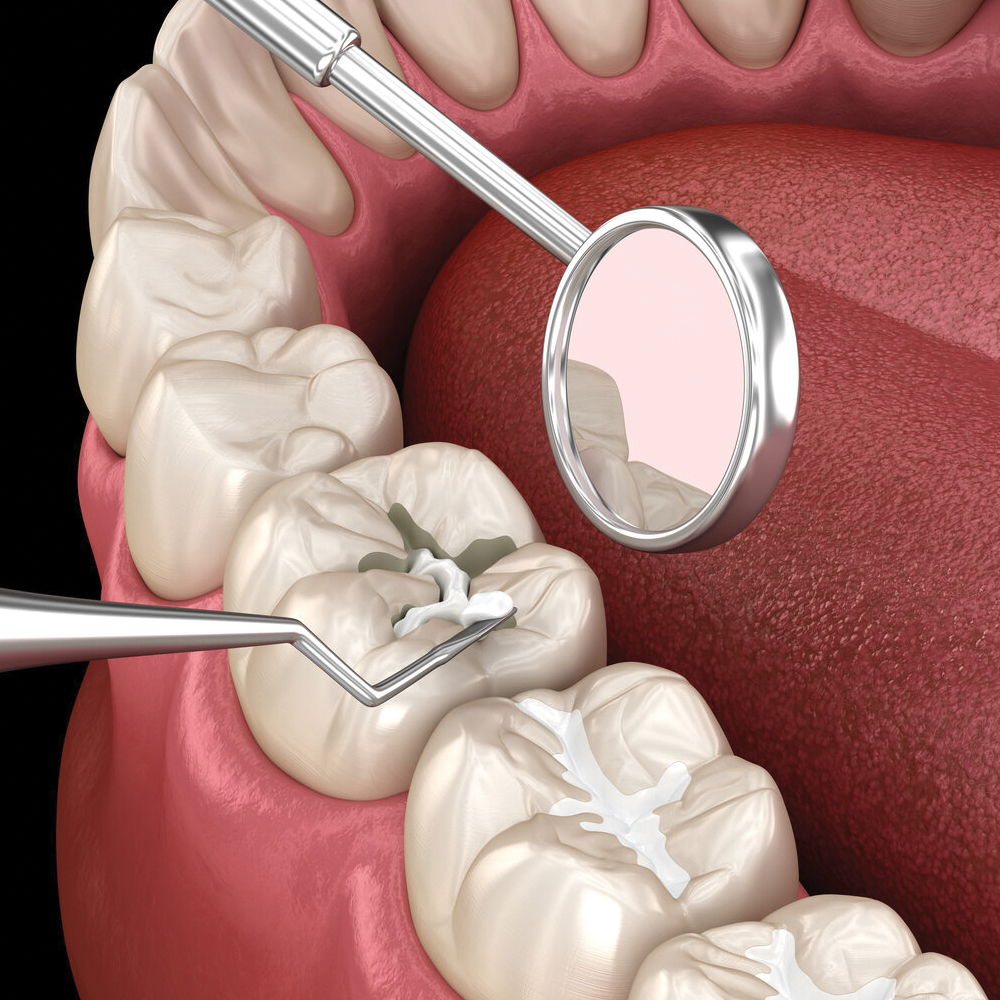
Diagnosing periodontitis involves a comprehensive dental exam, which includes a detailed evaluation of your oral health history, a clinical evaluation of your gums, and x-rays to assess bone loss. Your dentist can also measure the depth of the pockets between your teeth and gums using a probe. This process helps determine the severity of the disease and guides the appropriate treatment plan.
Request an appointment
Periodontitis Treatment Faq
How often should someone with Periodontitis visit the dentist for a check-up?
It is generally recommended that you visit the dentist every six months for regular checkups, but your dentist may recommend more frequent visits depending on your oral health needs.
Can periodontitis be genetic?
There is evidence to suggest that genetics may play a role in the development of periodontitis. If you have a family history of gum disease, it's important to be extra careful about your oral hygiene routine.
Can periodontitis occur even with good oral hygiene?
While good oral hygiene practices greatly reduce the risk of developing periodontitis, other factors such as genetics, smoking and certain medical conditions can contribute to its development.
What can you do about periodontitis?
The only solution is an immediate visit to the dentist to provide the appropriate treatment. Of course, for the treatment to be effective, continuous maintenance and optimal oral hygiene must be followed.
What is included in the Diagnosis and treatment of periodontitis?
The diagnosis of periodontitis usually involves a comprehensive dental examination, which includes a review of the patient's medical history, a thorough examination of the gums, and dental x-rays to assess the extent of bone loss. In some cases, additional diagnostic tests may be performed, such as a periodontal probe to measure the depth of the pockets.